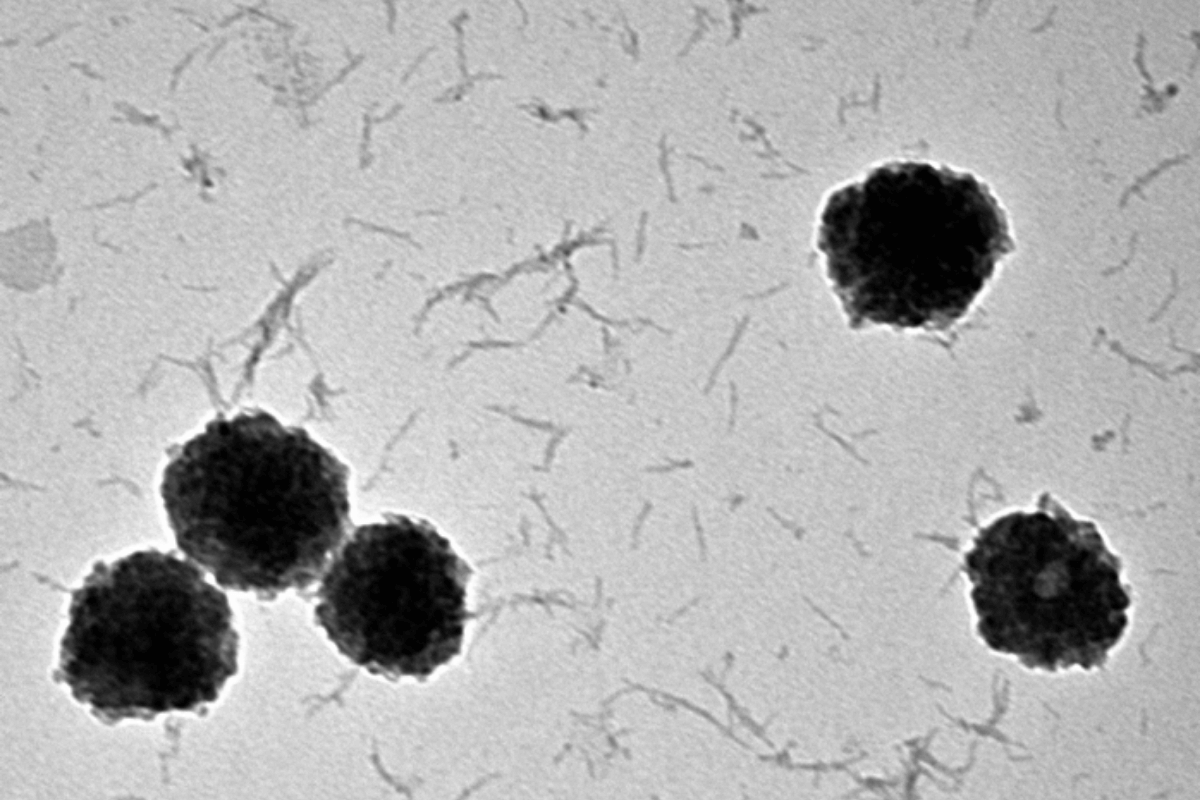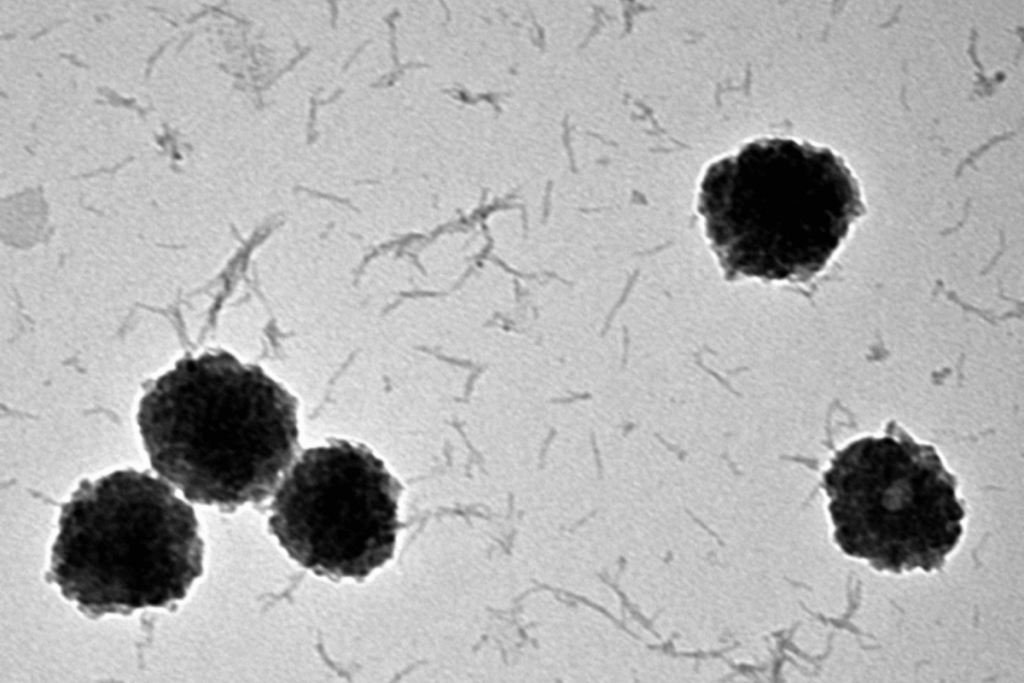
In a collaboration between UC Irvine and the National University of Singapore, researchers determined that the risk of developing cognitive impairment after chemotherapy may be attributable to differential plasma extracellular vesicles (EV) protein expression in breast cancer patients.
“This is the first time that any studies have demonstrated that these biomarkers might be associated with cognitive changes using human samples,” said Alex Chan, the Founding Chair of the Department of Clinical Pharmacy Practice at the UCI School of Pharmacy and Pharmaceutical Sciences. “In the long run, these findings have provided insights into how differentially expressed EV proteins may play a part in the pathogenesis of cognitive impairment in breast cancer patients.”
This study, published online in Biomarker Insights, is a collaboration between UCI School of Pharmacy and Pharmaceutical Sciences, the Department of Radiation Oncology at the UCI School of Medicine, the UCI Chao Family Comprehensive Cancer Center and the National University of Singapore. Charles Limoli and Munjal Acharya of the UCI Department of Radiation Oncology, who are experts in exosomes and EVs, have developed regenerative strategies to remediate from radiation-induced cognitive impairments.
Quinton Ng, a graduate student researcher studying for PhD in Pharmacological Sciences at UCI, is the second author on the study and continues to collaborate with the researchers in Singapore.
As a pilot study, this research used pooled samples to confirm the hypothesis of the link between EV protein expression and cancer-related cognitive impairment – also known as “chemobrain.”
“This study also illustrates the potential of using EV proteins as clinical biomarkers to predict and track the progression of cognitive impairment among breast cancer patients,” Chan said. “Scientists have also started using extracellular vesicle-based therapies to treat various disorders, and this could be a potential usage considering chemobrain lacks effective therapies at this time.”
The data from this initial research has warranted additional studies to evaluate the role of EVs in chemobrain.
“With our new collaborators at Radiation Oncology, together with the breast oncologists at the UCI Chao Family Comprehensive Cancer Center, we are planning to validate our findings with independent cohorts, including healthy controls,” Chan said. “We are launching a study soon among breast cancer patients to evaluate the findings in our pooled samples.”
Chan and his team also have a multicenter study ongoing in Singapore to determine the relationship between biomarkers and chemobrain in adolescent and young adult cancer patients.
“Eventually we will utilize the samples to evaluate the interaction of the harvested EVs with brain and blood-brain barrier cells,” Chan said, “with the goal to strengthen our understanding of the relationship between the EVs and cancer-related cognitive impairment.”